Case: When chest pain is not infarction – but aortic dissection
- Sep 28
- 2 min read
A 60-year-old man with known hypertension developed chest pain radiating to his left arm and shortness of breath in the morning. His symptoms worsened during a flight, and the aircraft was forced to make an emergency landing.
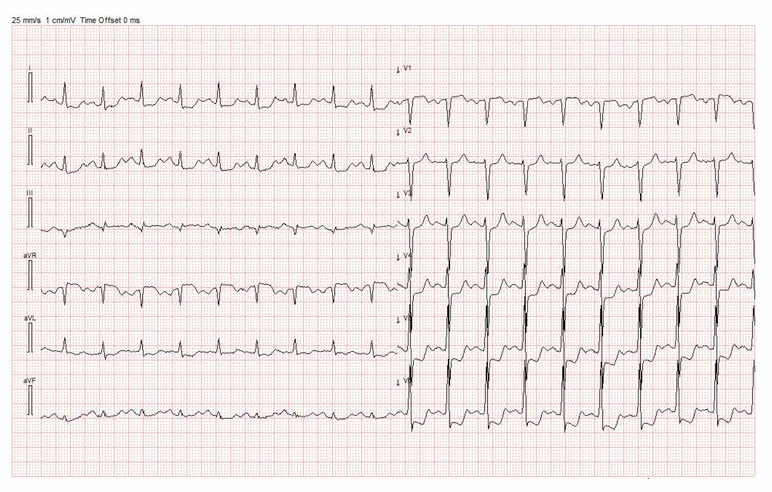
The prehospital ECG showed ST depressions in the precordial leads. He was in sinus rhythm with a heart rate of 120/min. Based on this, he was initially considered to have an acute myocardial infarction and was accepted for primary PCI.
On the way to the hospital, the patient deteriorated clinically with falling blood pressure, increasing oxygen demand (saturation 89% on 5 liters of oxygen), and lactate of 5 mmol/L.
Echocardiography
The examination revealed a hyperdynamic left ventricle without definite hypokinesia. The right ventricle appeared slender. Aortic regurgitation was present but difficult to quantify.
CT
Imaging demonstrated a type A aortic dissection with suspected involvement of the right coronary artery, along with signs of pulmonary congestion and edema. The patient was transferred urgently for surgery.
Why was this not an infarction?
The ST depressions were most pronounced in V4–V6, not in V2–V4 as would be expected in posterior infarction.
Patients with acute coronary syndrome are rarely in sinus tachycardia. Tachycardia may occur in cardiogenic shock, but this is typically associated with impaired left ventricular function or atrial fibrillation (7–10%).
In this case, the presence of sinus rhythm and a hyperdynamic left ventricle made infarction and cardiogenic shock less likely.
When the clinical picture does not fit perfectly, it is important to stop and reconsider. Differential diagnoses include pulmonary embolism and aortic dissection. The finding of aortic regurgitation in an acute setting should raise strong suspicion for dissection.
Learning points
ST depressions do not always indicate infarction – pay attention to pattern and localization.
Sinus tachycardia is unusual in acute coronary syndrome and should prompt consideration of other diagnoses.
A hyperdynamic left ventricle on echocardiography makes cardiogenic shock less likely.
Aortic regurgitation in the acute setting should immediately trigger suspicion of aortic dissection




Comments