top of page

BLOG
Healthcare Professionals


Cardiogenic Shock: Hemodynamics and Physiology Explained in Clinical Practice
How low cardiac output, elevated central venous pressure, and compensatory vasoconstriction shape treatment decisions in cardiogenic shock. (Part 2 in the Cardiogenic Shock series) Why This Article Is Necessary In Part 1 , we demonstrated how cardiogenic shock is frequently overlooked - particularly when blood pressure and early warning scores provide false reassurance. Many patients are already severely circulatory compromised long before hypotension develops. The goal of th
Faraz Afzal
6 days ago


Cardiogenic Shock With Normal Blood Pressure
Why Early Cardiogenic Shock Is Often Missed Cardiogenic shock is a life-threatening condition that is frequently recognized too late. One key reason is that patients do not always appear as we expect a patient in shock to appear. Blood pressure may be normal, vital signs only mildly abnormal — and the NEWS score surprisingly low. This article explains why this makes cardiogenic shock particularly dangerous , and which clinical signs should outweigh numbers alone . Key Learn
Faraz Afzal
Jan 26


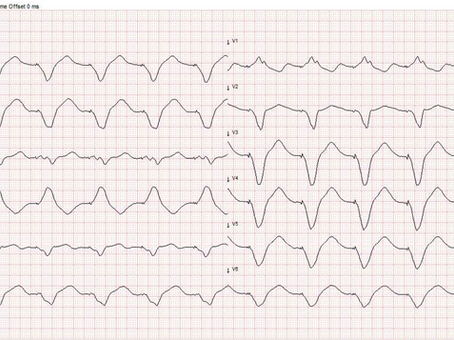
Shark-Fin Sign on ECG: A Life-Threatening STEMI Pattern Often Misinterpreted as Wide QRS
The shark-fin sign on ECG is a rare but extremely high-risk electrocardiographic pattern seen in acute myocardial infarction. It is most commonly associated with left main coronary artery occlusion or proximal LAD occlusion and carries a very high risk of cardiogenic shock, malignant arrhythmias, and cardiac arrest. Because the ECG appears to show an extremely wide QRS complex , the pattern is frequently misinterpreted by automated ECG algorithms and clinicians , leading t
Faraz Afzal
Jan 21

Circumflex Artery Myocardial Infarction: When Acute Coronary Occlusion Does Not Meet STEMI Criteria on ECG
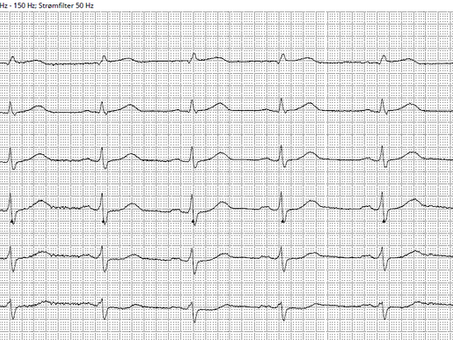
Acute occlusion of the left circumflex coronary artery (LCx) frequently causes transmural myocardial infarction without meeting classic STEMI criteria on the standard 12-lead ECG. This article explains why LCx infarctions are often misclassified as NSTEMI, illustrates a typical ECG pattern, and highlights key anatomical and electrophysiological principles that can prevent delayed revascularization. Prehospital ECG - standard leads Prehospital ECG - precordial leads Circumflex
Faraz Afzal
Jan 11


ICD (Implantable Cardioverter-Defibrillator): A Practical Clinical Guide for Healthcare Professionals
An implantable cardioverter-defibrillator (ICD) is a life-saving cardiac device, yet it is often perceived as complex in everyday clinical practice—particularly when explaining its function to patients. This article provides a clear, practical overview of how ICDs work, how they differ from pacemakers, and how they detect and treat ventricular arrhythmias using anti-tachycardia pacing (ATP) and shock therapy. Written for healthcare professionals, the goal is to translate adv
Faraz Afzal
Jan 7

Electrical Storm and Incessant Ventricular Tachycardia: A Practical, Step-by-Step Clinical Guide
Introduction Electrical storm and incessant ventricular tachycardia are life-threatening ventricular arrhythmias that require rapid, structured, and mechanism-based management. This practical clinical guide outlines a step-by-step approach to the assessment and treatment of electrical storm and incessant VT, based on current ESC, EHRA and AHA/ACC/HRS recommendations and real-world critical care experience. The article is written in collaboration with Dr Njord Nordstrand, Cons
Faraz Afzal
Dec 20, 2025

Slow Ventricular Tachycardia and Electrical Storm in a CRT-D Patient: A Clinical Case and Diagnostic Pitfalls - Part 1
Introduction Electrical storm and incessant ventricular tachycardia are among the most challenging conditions in acute cardiology, particularly in patients with structural heart disease and implanted cardiac devices. Rhythm diagnosis and selection of the correct treatment strategy can be difficult, and misclassification of arrhythmia may have serious clinical consequences. This case report describes the clinical course of a patient with ischemic cardiomyopathy and CRT-D, in w
Faraz Afzal
Dec 14, 2025


Why Hemoglobin Must Be Assessed Before STEMI Diagnosis and PCI
Chest pain and ST-segment abnormalities on ECG are among the most alarming findings in the emergency department. However, this case underscores an important principle: neither ST elevation nor widespread ST depression is synonymous with acute coronary occlusion. A thorough assessment of underlying physiology is essential to avoid misdiagnosis and inappropriate management. Case Presentation A man in his 70s presented with chest discomfort, dyspnea, and several weeks of deteri
Faraz Afzal
Nov 23, 2025


How a Pacemaker Works: A Complete, Clear, and Clinically Accurate Guide for Healthcare Professionals
A pacemaker is a small electronic device that keeps the heart beating at a safe and stable rhythm when the body’s own electrical system fails. In this complete, clinically accurate guide, you’ll learn exactly how a pacemaker works , when it is used , and what healthcare professionals should look for during a pacemaker check - including sensing, capture thresholds, and lead impedance. Whether you’re a clinician, student, or simply curious, this article provides a clear and re
Faraz Afzal
Nov 17, 2025


BRASH Syndrome
Case Presentation An 80-year-old man was found confused and somnolent at home. On EMS arrival, his blood pressure was 73/46 mmHg and heart rate fluctuated between 25 and 50 beats per minute. The ECG demonstrated a wide-complex bradycardia (rate 26). Atropine had no effect. He received intravenous adrenaline. On hospital arrival, the patient appeared pale, cold and hypotensive, with clinical signs of pulmonary edema and acute kidney injury. His creatinine was 260 µmol/L with
Faraz Afzal
Nov 14, 2025


Acute Chest Syndrome and Right Ventricular Failure
Case Presentation A man in his 40s from West Africa was admitted with diffuse pain throughout his body, including the chest. . On admission, he appeared clammy, in significant pain, and somnolent but easily arousable. Physical examination revealed no specific findings, but the patient appeared acutely ill and required supplemental oxygen due to hypoxia. ECG showed changes suggestive of pulmonary embolism. ECG (standard leads) - T-inversions in inferior leads. ECG findingings
Faraz Afzal
Nov 7, 2025


ECG-changes in pulmonary embolism vs. coronary occlusion - clinical case
A man in his 60s with a history of deep vein thrombosis and known factor V Leiden mutation was admitted with exertional, squeezing chest pain. The chest pain subsided, but the dyspnea persisted. On admission he was hemodynamically stable with a heart rate of 90/min and a blood pressure of 130/90 mmHg. He was asymptomatic at rest but became clearly dyspneic when walking to the bathroom. Sinusrythme. T-inversions in leads V1-V3. T-inversion i lead III. S-wave in lead 1. The ECG
Faraz Afzal
Oct 31, 2025


Case: Pre-excited Atrial Fibrillation in a Young Woman
Case Presentation A young woman was admitted with sudden-onset palpitations lasting approximately three hours before arrival. On admission, she was clammy, cold, and diaphoretic, and reported pre-syncopal episodes. Blood pressure was normal, and heart rate approximately 200 bpm. The admission ECG showed a wide-complexed, irregular tachycardia. Irregular wide-complexed tachycardia - Pre-excited AF Same ECG - More complexes (Standard leads) Same ECG - more complexes (precordial
Faraz Afzal
Oct 28, 2025


When the ECG Looks Dramatic – but the Heart Is Healthy
A previously healthy man in his 40s was admitted with chest pain considered atypical. The ECG showed ST elevations in aVL and in leads V2–V3, as well as ST depression in II, III, and aVF. T-wave inversions were also present in V3–V6. Despite these striking changes, the patient had preserved and tall R waves in the precordial leads. Echocardiography revealed no regional wall motion abnormalities, and troponin was as low as 4 ng/L. Because of the pronounced ECG changes and ches
Faraz Afzal
Oct 16, 2025
Widget Didn’t Load
Check your internet and refresh this page.
If that doesn’t work, contact us.
bottom of page
