Case: Pre-excited Atrial Fibrillation in a Young Woman
- Faraz Afzal
- Oct 28, 2025
- 2 min read
Updated: Jan 27
Case Presentation
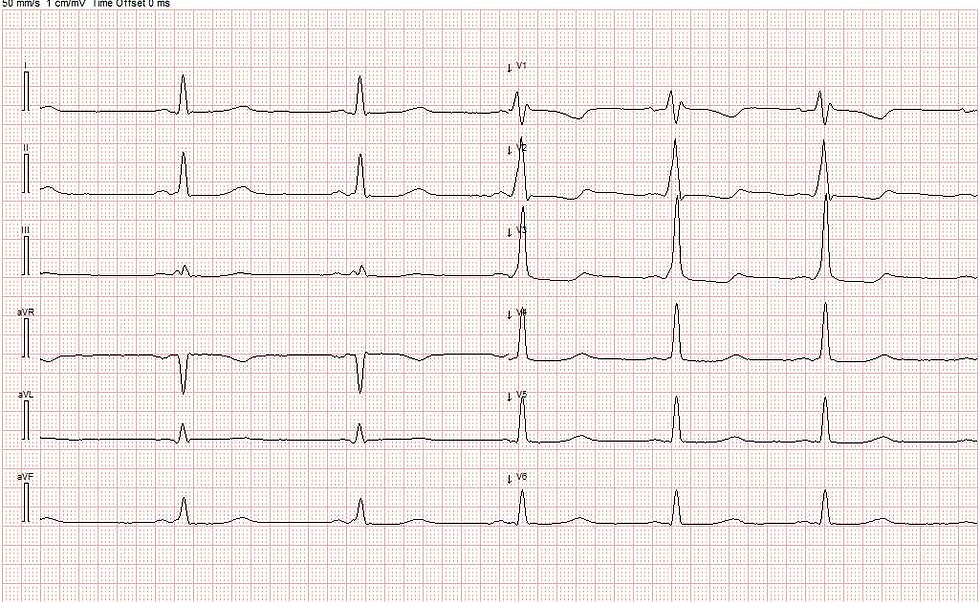
A young woman was admitted with sudden-onset palpitations lasting approximately three hours before arrival. On admission, she was clammy, cold, and diaphoretic, and reported pre-syncopal episodes. Blood pressure was normal, and heart rate approximately 200 bpm. The admission ECG showed a wide-complexed, irregular tachycardia.



ECG Interpretation
The rhythm was irregular, with variable R–R intervals and differences in QRS morphology.This pattern is characteristic of pre-excited atrial fibrillation (AF).
In typical AF, the AV node filters the rapid atrial impulses (around 600 per minute), allowing only a limited number to be conducted to the ventricles—usually resulting in a ventricular rate of 100–180 bpm. When an accessory pathway (Kent bundle) is present, atrial impulses can bypass the AV node and reach the ventricles directly without delay. This leads to an irregular broad-complex rhythm with varying QRS morphology, often due to fusion between impulses conducted via both the AV node and the accessory pathway.
Management and Course
The patient underwent electrical cardioversion to sinus rhythm. Post-conversion ECG demonstrated a short PR interval and a delta wave, consistent with ventricular pre-excitation or WPW (Wolff Parkinson Whites syndrome). Electrophysiological evaluation confirmed a left posterolateral accessory pathway.
Key Management Principles
Management of pre-excited AF requires particular caution.
Safest approach in the acute setting: Electrical cardioversion
Alternative: Flecainide for rhythm conversion in hemodynamically stable patients
AV node–blocking agents are contraindicated. These include:
Beta-blockers
Calcium channel blockers (verapamil, diltiazem)
Amiodarone
Adenosine
Blocking the AV node can result in all atrial impulses being conducted through the accessory pathway, depending on its conduction properties, which may precipitate ventricular fibrillation and sudden cardiac death.
Learning Points
Irregular broad-complex tachycardia should be considered pre-excited AF until proven otherwise.
Never administer AV node–blocking agents in suspected pre-excited AF.
Electrical cardioversion is the treatment of choice.
Flecainide may be considered for stable patients awaiting cardioversion.
Following stabilization, refer for electrophysiological evaluation and possible ablation of the accessory pathway.




Comments